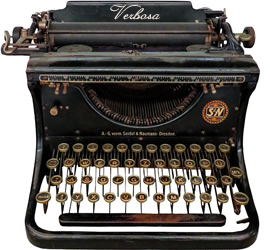
What is a Clinical Documentation Cheat Sheet?
A Clinical Documentation Cheat Sheet is a concise guide for healthcare professionals, streamlining patient encounter documentation. It provides a quick reference for recording accurate and comprehensive patient information efficiently, aiding in improved clinical workflows.
Purpose and Definition
The primary purpose of a clinical documentation cheat sheet is to provide a readily accessible, condensed summary of essential documentation elements. It serves as a quick reference tool, enabling healthcare providers to capture necessary patient information accurately and efficiently during clinical encounters. This tool aims to reduce documentation errors, promote consistency, and save valuable time for medical professionals. Essentially, it’s a streamlined guide to help ensure all critical aspects of a patient’s case are recorded correctly, supporting better patient care and legal compliance. This reference promotes complete and accurate records.
Key Components of Clinical Documentation
Key components include patient demographics, encounter details, medical history, treatment plans, and progress notes. These elements ensure comprehensive and accurate patient records, crucial for quality care.
Patient Demographics
Patient demographics are fundamental in clinical documentation, encompassing essential identifiers like the patient’s full name, age, gender, and contact details. Accurate recording of this information, including specific pronouns or identity preferences, is crucial for proper patient identification and communication. These details ensure correct matching of records and facilitate respectful and personalized care. Furthermore, complete demographic data is vital for administrative purposes, such as billing and insurance claims, highlighting its importance in the overall healthcare process. This information is the cornerstone of all patient records, underpinning effective medical documentation.
Encounter Details
Encounter details are a vital part of clinical documentation, capturing the specifics of each patient interaction. This includes the date, time, and location of the encounter, alongside the type of visit, be it an office appointment, hospital admission, or telehealth consultation. The healthcare professional involved must also be clearly identified. Documenting the reason for the encounter, whether a routine check-up, a specific complaint, or a follow-up, provides context for the medical information recorded. Accurate encounter details enable a clear timeline of patient care, which is essential for continuity and effective healthcare management.
Medical History and Assessment
The medical history and assessment section of clinical documentation is crucial for understanding a patient’s overall health. This includes recording past medical conditions, surgeries, allergies, and current medications. A thorough assessment involves documenting the patient’s presenting symptoms, a physical examination, and any relevant findings. It also details the subjective complaints reported by the patient and the objective observations made by the healthcare provider. The medical history and assessment provides the baseline information from which to create treatment plans and monitor patient progress, essential for comprehensive and effective care.
Treatment Plans and Interventions
This section outlines the specific strategies designed to address the patient’s health issues. Treatment plans should include clear goals, specific interventions, and any necessary referrals. Interventions can include medication orders, therapies, surgical procedures, or lifestyle modifications. It is essential to document the rationale for chosen treatments, and any discussions with the patient regarding these plans; This also includes documenting patient responses to interventions and any adjustments made to the plan based on the patient’s progress. Comprehensive documentation of treatment plans and interventions ensures continuity of care and facilitates informed decision making by all care providers.
Progress Notes and Outcomes
This area focuses on the ongoing evaluation of the patient’s condition and the effectiveness of the treatment plan. Progress notes should detail the patient’s response to interventions, any changes in symptoms, and the results of any tests. It’s crucial to document both positive and negative outcomes, noting any complications or adverse events. The notes should reflect any adjustments made to the treatment plan based on the patient’s progress. These notes should include the date and time of the observation, and be concise and objective. This section is vital for monitoring the patient’s trajectory and ensuring quality care.
Importance of Accurate Documentation
Accurate documentation is vital for patient care, legal protection, and proper billing. It ensures clear communication among providers, facilitates effective treatment, and supports ethical practice.
Legal and Ethical Considerations
Clinical documentation serves as a legal record of patient care, making accuracy paramount. Incomplete or inaccurate documentation can lead to legal repercussions and ethical breaches. Healthcare providers must adhere to established guidelines to ensure patient information is properly documented, protecting both the patient and the provider. These guidelines dictate the requirements for medical documentation, maintaining uniformity and compliance. Proper documentation also demonstrates a commitment to ethical practice, reflecting the quality of care provided and respecting patient rights. It’s crucial to understand the legal and ethical implications of clinical documentation to avoid potential issues.
Impact on Patient Care
Accurate clinical documentation directly impacts the quality of patient care. It facilitates clear communication among healthcare team members, ensuring continuity and coordination of treatment. Thorough records provide a comprehensive understanding of a patient’s condition, enabling informed decision-making and personalized care plans. Incomplete or inaccurate documentation can lead to misdiagnosis, delayed treatment, and potentially adverse outcomes. Proper documentation also helps track patient progress, allowing providers to evaluate the effectiveness of interventions and make necessary adjustments. Ultimately, high-quality clinical documentation contributes to improved patient safety, outcomes, and overall satisfaction, forming the bedrock of patient care.
Billing and Reimbursement
Clinical documentation serves as the foundation for accurate billing and reimbursement. Detailed and precise records justify the medical services provided, ensuring healthcare providers receive appropriate payment. Insufficient or inaccurate documentation can lead to claim denials, reduced reimbursements, and potential financial losses for healthcare facilities. Furthermore, compliance with coding guidelines and payer requirements relies heavily on the information documented in patient records. Clear documentation of medical necessity, procedures performed, and patient conditions is essential for supporting claims and avoiding audits. Thus, thorough clinical documentation is not only vital for patient care but also for the financial stability of healthcare organizations.
Improving Documentation Practices
Enhancing documentation involves using templates and checklists, leveraging technology like EMRs, and understanding clinical guidelines. These strategies promote accuracy, consistency, and efficiency in recording patient information.
Using Templates and Checklists
Implementing templates and checklists can significantly improve clinical documentation. Templates offer a structured format, ensuring all necessary data points are captured consistently. Checklists act as a reminder, guiding healthcare providers through essential documentation elements. This approach reduces the risk of omissions and enhances the clarity of notes. By standardizing the documentation process, templates and checklists promote efficiency, minimize errors, and contribute to better overall patient care. They provide a framework, making the documentation process less burdensome and more reliable, leading to more thorough and accurate records.
Leveraging Technology (EMRs)
Electronic Medical Records (EMRs) are powerful tools for improving clinical documentation. EMRs facilitate efficient data entry, storage, and retrieval, allowing healthcare providers to easily access patient information. Features like pre-populated fields, drop-down menus, and automated prompts help standardize documentation and reduce errors. EMRs also enable seamless sharing of patient data amongst healthcare teams, enhancing communication and collaboration. Moreover, EMRs can integrate with clinical decision support systems, providing real-time guidance to providers. By leveraging these technological capabilities, healthcare professionals can create more thorough, accurate, and easily accessible clinical documentation.
Understanding Clinical Documentation Guidelines
Clinical documentation guidelines are essential for maintaining uniformity and compliance within medical records. These guidelines specify the requirements for accurate and comprehensive documentation, ensuring that practitioners record all necessary information. Understanding these guidelines helps healthcare professionals adhere to legal and ethical standards while also improving the quality of patient care. They dictate how to document patient encounters, including assessments, treatments, and progress notes. These guidelines often outline specific data points required, ensuring consistent and thorough record-keeping across different healthcare settings. Furthermore, these guidelines help practitioners avoid potential legal and billing issues associated with incomplete or inaccurate documentation.

Quick Reference Guide Formats
Quick reference guides for clinical documentation can vary, including checklists, flowcharts, and tables. The format should be concise and easy to use, ensuring quick access to needed information.
Tips for Attractive Layouts
For an effective quick reference guide, prioritize a clean and uncluttered layout. Use clear headings and subheadings to organize information logically. Employ bullet points or numbered lists for easy scanning. Incorporate visual cues like bold text or color-coding to highlight key details. Ensure sufficient white space to prevent visual overwhelm. Choose a legible font and appropriate font sizes. Consider a consistent design throughout the document for a professional appearance. A well-structured and visually appealing guide enhances usability and encourages regular use by healthcare professionals.
Clinical Documentation Improvement (CDI) Programs
CDI programs are vital for ensuring accurate, complete, and compliant clinical documentation. These programs aim to improve the quality of patient records, supporting better care and appropriate reimbursement.
Role of CDI in Organizations
Clinical Documentation Improvement (CDI) programs play a crucial role in healthcare organizations by enhancing the accuracy and completeness of patient records. They help ensure that documentation reflects the care provided, supporting appropriate coding and billing. CDI specialists work with providers to clarify diagnoses and procedures, leading to better data quality. This, in turn, impacts patient care outcomes, facilitates effective communication, and minimizes legal risks. Furthermore, CDI programs contribute to improved clinical outcomes and financial stability by accurately capturing the severity of patient conditions.
Resources for Clinical Documentation
Healthcare professionals can utilize various resources, including reference guides, manuals, and online tools, to enhance their clinical documentation practices and ensure accuracy and compliance with standards.
Reference Guides and Manuals
Numerous reference guides and manuals are available to support healthcare providers in maintaining high-quality clinical documentation. These resources often include detailed explanations of documentation requirements, best practices, and legal considerations. They may also provide specific examples and templates to help clinicians record patient information accurately and efficiently. Additionally, some guides focus on specific areas, such as coding, billing, and compliance, ensuring that all aspects of documentation are covered. These materials can be found in print, online, and through professional organizations, offering a wealth of knowledge for improving documentation practices.